|
Reproductive Health Care During the COVID-19 Pandemic
Amidst the current COVID-19 public health emergency, patients continue to face many of the same sexual and reproductive health issues they always have (Figure 1). Each year in the U.S. there are nearly 47 million women using contraception, 20 million new cases of sexually transmitted infections (STIs), 3.8 million births, 1 million pregnancy losses, 6.5 million women with endometriosis, 862,000 abortions, and 94,000 women newly diagnosed with gynecologic cancer. This is not to mention the millions of patients each year who access preventive services for reproductive health (e.g. STI and cancer screenings, HPV vaccinations). The difference now, however, is that much of this care is being delayed due to the COVID-19 emergency.
After decades of public health initiatives urging people to not delay or forgo many types of care, we are now experiencing a paradigm shift in response to COVID-19. Facing extraordinary circumstances, the U.S. government, states, health centers and providers have been tasked with determining which health care services are “essential,” and which are “elective,” or “non-urgent” thereby influencing what care is available to patients at this time. Beginning in March 2020, guidance from the CDC urged providers to postpone non-urgent outpatient visits and preventive health care, if it was not able to be performed via telehealth. Additionally, both the CDC and CMS recommended postponing “elective” and “non-essential” surgeries and procedures, using a tiered framework that balanced how severe and time-sensitive a patient’s needs were, with the tradeoffs associated with in-person care (e.g. coronavirus exposure, depletion of PPE). As of May 21, 2020, the CDC removed said language regarding delaying non-urgent visits and “elective” procedures from their published guidance. During that time however, dramatic decreases were seen in patients seeking reproductive health care, and health care more generally.
A study by Strata Decision Technology of 228 hospitals across 40 states found patient encounters for various reproductive health services showed large decreases compared to the year prior (Figure 2). The largest drops in patient volume were seen for preventive health services, infertility care, and contraception, with smaller, but still sizable decreases in encounters for gynecologic cancer and pregnancy. A study by IQVIA similarly showed an 83% decline in the number of pap smears in April compared to February 2020.

Figure 2: Patient Visits at Hospitals and Doctors’ Offices Plummeted in the Initial Months of the COVID-19 Pandemic
What have medical professional societies said about delaying reproductive health care?
Various medical societies have issued guidance to help providers decide which reproductive health services necessitate prompt, in-person care, which may be suitable for telehealth, and which may be delayed altogether (Appendix). In general, most pregnancy-related services have been considered essential (prenatal care, labor and delivery, ectopic pregnancies, pregnancy loss, abortions), as well as most treatments for gynecologic cancer. Meanwhile, some methods of contraception that require in-person care (e.g. sterilization, IUD removal), as well as most preventive health care (e.g. STI and cervical cancer screening, HPV vaccines) have been recommended to be postponed. The Society for Family Planning’s guidelines emphasize use of telehealth to assess if an in person visit is required, or if contraception can be provided and managed through a virtual visit. That said, recommendations for care have been changing rapidly during the course of the COVID-19 emergency; for example, as of March 2020, the American Society for Reproductive Medicine recommended cancelling all new infertility treatments and diagnostic procedures, but relaxed these recommendations as of May 2020.
What decisions have state governments made?
Some states have specifically deemed certain reproductive health services essential or non-essential. This is most common when it comes to abortion services. At least 12 states (AK, AL, AR, IA LA, MI, OH, OK, TN, TX, WV) issued policies to suspend abortion during the COVID-19 emergency; most bans are not in effect however due to ongoing or resolved litigation, or states lifting restrictions on “non-essential” services. Meanwhile, 5 states (MA, NJ, NM, VA, WA) included language in their executive orders or public health guidance to clarify that abortion is considered essential, or to explicitly protect the “full suite of family planning services.”
For pregnancy-related care, New Mexico and Tennessee have specifically excluded pregnancy-related visits or procedures from their definition of “non-essential” care. Regarding gynecologic cancer, a handful of states clarify that postponement of elective procedures does not apply if there is a risk of cancer advancing or spreading (AR, IA) or if the treatment is to remove a cancerous tumor (FL, NM, TN, WA). Meanwhile, Massachusetts specifically included colposcopy (to detect cervical cancer) and endometrial biopsies (to detect uterine cancer) as examples of “nonessential, elective” procedures.
More commonly however, states have not specified certain procedures or diagnoses in their executive orders regarding COVID-19. Rather, states more broadly defined “non-essential” procedures as those which can be safely postponed for a certain amount of time without risking serious harm to the patient. As of mid-April 2020, 32 states had issued formal orders to postpone so-called “elective” and “non-essential” surgeries and procedures, but by mid-May 2020, the majority had rolled back these restrictions to allow some procedures to continue, under certain conditions. At the federal level, in June 2020 CMS recommended that patients should not further delay preventive care such as cancer screenings and vaccinations. As the COVID-19 pandemic evolves in the months to come, some regions with recurrent outbreaks of SARS CoV2 will likely have to consider reinstating restrictions on “non-essential” services.
What could be the impact of delays in care?
For years, public health officials and providers have urged the public to actively seek reproductive health care, as we know the negative health consequences that may result from not doing so. We know that limited access to contraception puts women at risk for unintended pregnancies, while undetected and untreated STIs can lead to complications like infertility, pelvic inflammatory disease and ectopic pregnancies. We know that forgoing prenatal care may result in poor maternal and infant outcomes, and that halting time-sensitive fertility care may reduce the chance for family building for the 10-15% of couples with infertility. Meanwhile, untreated conditions like endometriosis and fibroids can result in significant morbidity, and delays in gynecologic cancer diagnosis and treatment could mean cancer progression and increased mortality. We also know that even when reproductive health conditions are not life-threatening, they threaten to reduce one’s quality of life and overall wellbeing, and therefore warrant care and attention.
Health systems and providers have been forced to adapt to the evolving landscape of the coronavirus pandemic, and most have quickly adopted telehealth solutions in order to continue to see patients; many reproductive health care services can be delivered via telehealth, including prescription of hormonal contraception and many prenatal/postpartum visits. There have also been innovations during the pandemic in using telehealth for medication abortion, and to assist patients in IUD self-removal and self-administered Depo-Provera injections. That said, several services still require in-person care, including several of the most effective methods of contraception (e.g. sterilization, IUD and implant placement), several preventive services (e.g. HPV vaccination, cervical cancer screening), procedural abortions, and the host of procedures and surgeries used to diagnose and treat many gynecologic conditions (e.g. infertility, endometriosis, gynecologic cancers). These services requiring in-person attention are at risk of delay during the COVID-19 pandemic.
Will patients who have delayed care return?
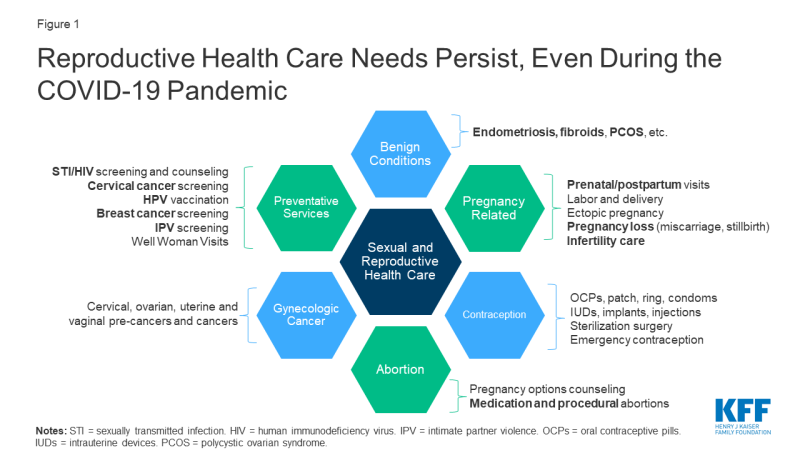
Data from the KFF May 2020 Health Tracking Poll reveal more than half of US women reported they or a family member have skipped or postponed medical care due to the coronavirus outbreak. A majority of those who delayed care also reported the condition did not get worse in that time, and that they planned to seek care within the next 1 to 3 months (Figure 3). Therefore, it seems as if most plan to return to care in the near future. That said, many people also remain fearful of accessing in-person health services; a Gallup poll (conducted March 28 to April 2, 2020) showed 88% of US women reported being very or moderately concerned about being exposed to the novel coronavirus at a doctor’s office or hospital; this dropped to 70% when the poll was conducted again from May 14 to 24, 2020. Patients may also forgo care due to cost, as over half of the workforce has lost their jobs or wages, and some may have subsequently lost their health insurance.
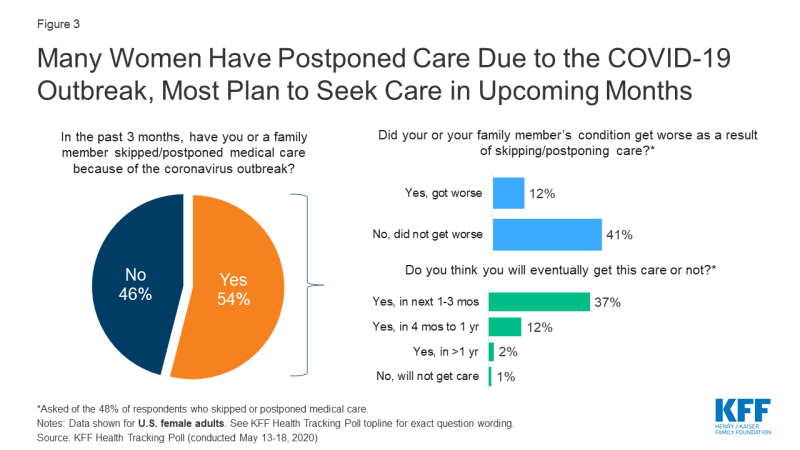
Figure 3: Many Women Have Postponed Care Due to the COVID-19 Outbreak, Most Plan to Seek Care in Upcoming Months
When patients return to care, will the health care system be ready?
When and if patients decide to seek in-person care, it is important to note that providers may be functioning at reduced clinic capacity as compared to before the coronavirus outbreak. A survey of primary care providers from 48 states (conducted May 22-26, 2020) revealed that many practices are struggling financially; 14% of provider’s practices were still temporarily closed, and 77% reported net-negative revenues in April 2020. Many have had to furlough or layoff staff, and were uncertain if they would remain open in the weeks to come. It remains to be seen if the financial impact to medical practices will still allow these sites to function at pre-COVID-19 patient volumes in the months to come. This may be particularly difficult for publicly-funded family planning clinics, given existing funding challenges related to changes in Title X.
Looking Forward
Even amidst the coronavirus pandemic, millions of patients continue to need quality sexual and reproductive health care in the U.S. While most providers have shifted to telehealth in an attempt to maintain care, many reproductive health conditions that have been deemed “non-essential” require in-person evaluation and treatment, and therefore patients have experienced delays in this care. As the U.S. looks to move into the next phase of the COVID-19 emergency, states and health systems are deciding when it is appropriate to resume provision of these in-person, “non-essential” health care services. While many have loosened restrictions, a second wave of the pandemic or infection hotspots may force providers again to restrict in-person care. As public leaders and officials monitor the capacity of our health systems to respond patient needs during the COVID-19 pandemic, they will also continue to be faced with difficult decisions regarding whether again to delay many reproductive health care services that are critical to women’s health.
Appendix"care" - Google News
June 24, 2020 at 08:17PM
https://ift.tt/2BA7lD2
Potential Impacts of Delaying “Non-Essential” Reproductive Health Care - Kaiser Family Foundation
"care" - Google News
https://ift.tt/2N6arSB
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini














0 Response to "Potential Impacts of Delaying “Non-Essential” Reproductive Health Care - Kaiser Family Foundation"
Post a Comment