Primary care practices provide most mental health services that patients receive, in place of, or in collaboration with, mental health specialists. They are also the most common source of preventive services, care coordination, and partnership with other sectors outside health care, such as social services, that are necessary to achieve health equity. The US grossly underfunds primary care and restricts payment to a narrow set of services not reflective of what patients need and not in accord with how high-performing primary care practices work.
We propose a dramatic redesign of Medicare payment for current and new primary care functions and increased payment levels. We can no longer afford to wait for pilot programs to generate change at scale. A decade of experimentation with medical home and value-based payment models points the way to permanent solutions, captured in recent recommendations from the National Academes of Science, Engineering, and Medicine.
The Most Powerful Medicare Platform For Payment Innovation
A bold approach to improving mental health and addressing inequity at a large scale would focus on primary care payment in the Medicare Shared Savings Program (MSSP). This would provide a solid chassis on which to ultimately integrate multiple payment innovations into Medicare’s flagship value-based payment program.
The MSSP, which offers accountable care organizations (ACOs) financial rewards to deliver high-quality care and contain total spending, is a permanent program reaching 11 million Medicare beneficiaries, with regulatory flexibilities explicitly allowing the Centers for Medicare and Medicaid Services (CMS) to make changes in payment structures and waive other existing Medicare requirements. The most successful ACOs have been built upon a strong base of primary care. CMS officials have committed to use the MSSP to synthesize and magnify successful features from multiple value-based payment programs. These factors make the MSSP a powerful vehicle for redesigning primary care payment with a focus on improving health.
Use Hybrid Population-Based And Fee-For-Service Payment To Rejuvenate Primary Care
We envision a voluntary payment option available to MSSP ACOs, structured as a hybrid of population-based payments (PBPs) and fee-for-service. PBPs would take the form of a monthly, per-beneficiary amount and would account for most of a provider’s payment. PBPs would give practices flexibility to optimize the mix of compensated services they currently offer and support diverse activities practices perform but are not paid for now, such as team-based care, emails, and phone calls. Desirable services that a minority of practices deliver, such as hospital visits and health-critical services that are important for all patients to receive, such as immunizations, would continue to be paid fully through fee-for-service to encourage their delivery.
We recognize that moving entirely to per-beneficiary, per-month PBPs risks eliminating the incentive fee-for-service payments provide for practices to conduct office visits when appropriate and to submit the accurate encounter data that CMS needs for patient attribution. Therefore, we propose dividing payment for individual office visits, with the larger portion as part of the PBP and the remainder as a per-visit payment at a single code level for all visits. The Primary Care First model pioneered use of a single office visit code. This proposal leverages that concept, but with methodologic refinements such as the inclusion of telehealth services, designed to promote equity and integrative primary care. The office visit payment should approximate marginal costs to practices of providing an additional visit to neutralize current incentives to increase profits by increasing volume. Exhibit 1 summarizes the proposed payment structure.
Exhibit 1: Summary of proposed hybrid payment for primary care practices in the Medicare Shared Savings Program
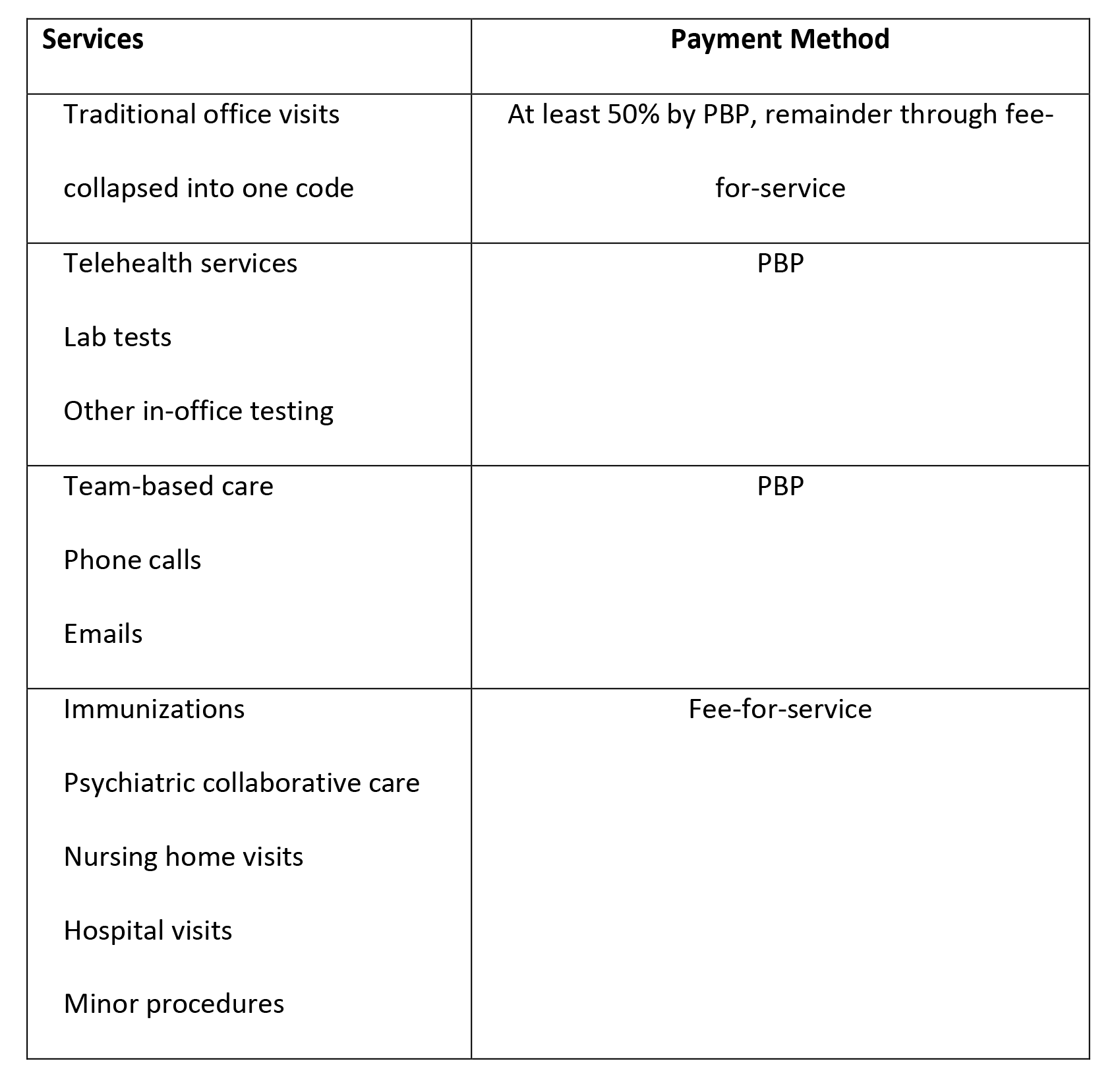
Source: Authors’ analysis.
Payment levels for the PBP portion should reflect significant increases over historical prices for the relevant services, to adequately compensate primary care providers and allow them to invest the time necessary to address patients’ mental health and social needs. Data on the percentage of a typical provider’s workday spent on uncompensated activities, the well-documented legacy of relative undervaluation of primary care services in the Medicare Physician Fee Schedule (MPFS), and growing expectations on primary care cumulatively suggest this increase should be at least 30 percent.
Key Adjustments Account For Patient Complexity And Support Savings
CMS should adjust PBPs for patient complexity using a primary care-specific method, focusing on variation in spending on primary care work rather than total costs of care. Costs for hospitalizations, postacute care, and other services not included in the PBP should be excluded. PBP amounts should also be adjusted for beneficiaries’ socioeconomic status, similar to adjustments proposed in the ACO REACH model.
The ACO is accountable for total costs of care and would take on responsibility for a small number of quality metrics to guard against stinting on care. These metrics would focus on mental health, equity, and elements of patient experience of particular salience today, such as patients’ trust in their provider and effective care coordination.
Because some services may be “invisible” to patients, such as practices’ reaching out to social service agencies for patients with complex needs, we suggest using MSSP’s waiver authority to remove patient cost sharing for the PBP. Beneficiaries would have a hard time understanding extra monthly charges for services they were not aware of.
Increasing payment over historical levels and waiving cost sharing would result in higher spending, and the MSSP authority requires that any new payment arrangement be budget neutral. One solution would be to initially offer hybrid payment only to ACOs that take on two-sided risk—that is, agree to share losses as well as gains with CMS – because those ACOs would have to generate sufficient total spending reductions to cover the costs of additional primary care payments before they can qualify to receive shared savings. An alternative would be to offer hybrid payment to all ACOs but only reconcile and require repayment of any overspending after at least three years of performance. This would allow ACOs time to generate savings to cover the increased spending.
Assuming PBPs are 30 percent higher than historical levels, and that primary care services currently account for less than 3 percent of Medicare expenditures, additional payments would be roughly equivalent to only 1 percent of an ACO’s total expected financial target. The value of waived cost-sharing would be less. While the additional spending would not be insignificant, we believe this is a level of increased accountability that many ACOs would be willing to take on for the opportunity to recruit more primary care providers by offering higher payment and investment in infrastructure to help them improve patients’ health.
Focus On Independent Physicians To Drive Healthier Market Dynamics
While all ACOs could benefit from hybrid payment, CMS should initially offer it only to ACOs composed of independent practices—those not employed by or contracting with hospitals in clinically integrated networks. Targeting ACOs with independent practices would have the desirable effect of giving practices an incentive to remain independent, dampening vertical market consolidation that has contributed to rising health care prices. It would also give financially struggling practices an alternative to acquisition by private-equity firms or health systems. Physician-led ACOs have also shown better savings performance, on average, than ACOs that include hospitals. Favoring physician-led ACOs initially might also encourage more practices to join or form new ACOs and increase MSSP participation.
Don’t Limit Primary Care Payment Innovation To What Might Generate Short-Term Savings
Historically, CMS has adopted permanent fee-for-service innovations for primary care through the MPFS and tested population-based and medical-home approaches through the Innovation Center. This has generated important lessons, such as the value of upfront infrastructure payments and the peer-to-peer learning, but not savings, possibly because base payment to clinicians has remained fee-for-service. Also, Innovation Center models that invest more in primary care are challenged to generate short-term Medicare savings that would qualify them for scaling, and those that do not and/or offer small PBP amounts are not true tests of PBP-heavy hybrid payments.
CMS recently announced its intent to scale the ACO Investment Model to offer upfront payments for care management infrastructure and broaden the types of ACOs that would qualify. The Innovation Center announced the ACO REACH model that emphasizes PBPs and may plan additional primary care models. Using the MSSP to innovate primary care payment at scale would complement these strategies and drive important market changes toward better population health.
Authors’ Note
This work was funded by a grant from the Commonwealth Fund. Sean Cavanaugh is an executive at Aledade, Inc., which supports independent primary care practices in performing as accountable care organizations.
"care" - Google News
October 17, 2022 at 07:13PM
https://ift.tt/Yqb3Bsz
Using The Medicare Shared Savings Program To Innovate Primary Care Payment - healthaffairs.org
"care" - Google News
https://ift.tt/7sDA6YC
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini














0 Response to "Using The Medicare Shared Savings Program To Innovate Primary Care Payment - healthaffairs.org"
Post a Comment